48 M with pain abdomen and lower back pain since 1 week
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
48 M resident of suryapet, farmer by occupation came to the opd with c/c of lower back pain and pain abdomen since 1 week
HOPI
patient was apparently asymptomatic 1 week ago and then he developed pain abdomen which was a dragging pain in nature, relieved on medication. no aggravating or relieving factors. he also developed lower back pain since a week which is relieved on medication. the patient also complained of facial swelling since 2 days
past history
n/k/c/o dm, tb, epilepsy, htn,
15 years ago he was admitted in the hospital for 2-3 days due to jaundice and then he was discharged & asked to take medication.
personal history
sleep - adequate
bowel and bladder - regular
appetite - normal
addictions - bidi and cigarette smoking since 20 years ago
alcohol 1 quarter daily since 20 yrs
he stopped since an year because he had pain abdomen and sob
family history - not significant
daily routine -
he wakes up at 4-5 am and then milks the cows
he then attends to some farm work agriculture work
at around 9 am he eats rice with pickle or curry and then works again in the fields and drives a tractor
at around 10 pm he eats jawar roti and goes to bed.
he hasn’t been able to work since five days because of the pain.
general exam
patient is conscious coherent and co operative
moderately built and nourished
pallor- absent
icterus - mild
clubbing - absent
cyanosis - absent
generalised lymphadenopathy- absent
pedal edema - absent
vitals
Temp: 98.6F
pulse rate: 65 bpm
Blood pressure - 110/70 mm hg
Respiratory rate: 16 cpm
Systemic examination
cvs -
no thrills,
no cardiac murmurs,
S1 and S2 sounds heard
rs -
dyspnoea is absent,
position of trachea is central,
no wheeze,
vesicular breath sounds present
abdomen -
normal in shape,
no tenderness,
no palpable mass,
hernial orifices are normal,
no bruits or free fluid,
liver and spleen are not palpable,
bowel sounds are present.
cns -
conscious
speech is normal
kerning's sign is negative
brudzinskis sign negative
rombergs sign negative
cranial nerves, motor system, sensory system are all intact and normal.
provisional diagnosis - alcoholic liver injury
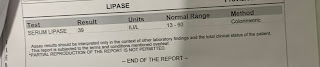
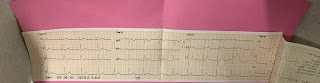
investigations -










Comments
Post a Comment