80 Y/O M WITH SHORTNESS OF BREATH AND EPIGASTRIC PAIN
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
An 80 year old male from orangudam, farmer by occupation, came to the OPD with chief complaints of shortness of breath since 1 year, epigastric pain and discomfort after eating food since 6 months, diminished vision in both eyes since 1 year and bilateral knee pain since 2 years.
History of presenting illness
Patient was apparently asymptomatic 1 year ago and then he developed shortness of breath, insidious in onset and gradually progressed from grade I to grade II. No paroxysmal nocturnal dyspnoea, no orthopnea, no diurnal and seasonal variations. Epigastric pain and discomfort after eating food since 6 months and especially after eating spicy food.
History of past illness
k/c/o hypertension since 10 years and on medication since 1 year)
n/k/c/o diabetes mellitus, hyper or hypothyroidism, asthma, CAD, epilepsy and tuberculosis.
Family history
not significant
Personal history
appetite is normal
bowel and bladder movements are regular
no known allergies
habit of alcohol consumption once monthly occasionally since 10 years.
no habit of tobacco use
General examination
Patient was conscious, coherent and co-operative,
No Icterus, Cyanosis, Koilonychia, Generalised lymphadenopathy, Pedal edema.
Vitals
Temperature - Afebrile
Pulse rate - 98 bpm
Respiratory rate - 18 cpm
BP - 190/100 mm of Hg
SpO2 - 98% at room atmosphere
GRBS - 148 mg/dL
Systemic examination
cvs -
no thrills,
no cardiac murmurs,
S1 and S2 sounds heard
rs -
dyspnoea is present,
position of trachea is central,
no wheeze,
vesicular breath sounds present
abdomen -
scaphoid in shape,
no tenderness,
no palpable mass,
hernial orifices are normal,
no bruits or free fluid,
liver and spleen are not palpable,
bowel sounds are present.
cns -
conscious
speech is normal
no neck stiffness, no kerning's sign
cranial nerves, motor system, sensory system are all intact and normal.
reflexes -
RT. LT
biceps 2p. 2p
triceps 2p 2p
supinator 1+ 1+
knee 2p. 2p
ankle 1+ 1+
cerebellar signs -
no finger nose incoordination
no heel knee incoordination
gait is normal
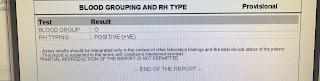
Investigations-









Comments
Post a Comment